現在位置
Last updated on April 1, 2025.
The text is from here.
Rehabilitation of stroke and neurological disorders
Rehabilitation of Stroke
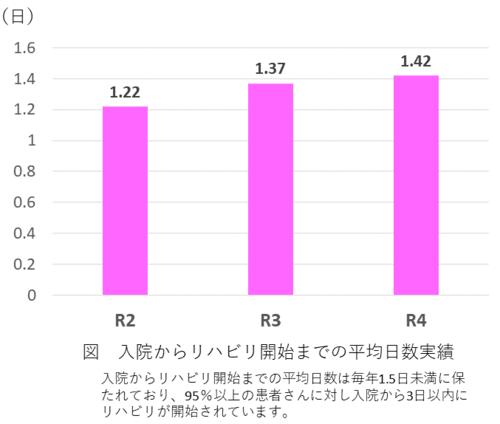
Early rehabilitation utilizing acute medical functions
- Rehears will begin within 3 days of hospitalization for acute stroke.
- In cooperation with doctors and nurses, we aim to stabilize the whole body condition, establish a daily rhythm, and leave the bed early.
- One-on-one (one-on-one) training to restore functions from an early stage.
Physiotherapy
From the early stage of the onset, a physiotherapist visits the sick room and performs exercise on the bed, sitting on the bed, and standing practice according to the patient's condition, while considering safety management. .
Occupational therapy
From the early stage of the onset, occupational therapists visit the hospital room and practice using paralyzed hands. We also support you so that you can work on your own.
Rehabilitation at bedside
Consistent rehabilitation from acute phase to convalescent phase
- It is possible to enter the rehabilitation ward from the acute ward without transfer.
- The convalescent rehabilitation ward is undergoing rehabilitation 365 days a year.
- With one-on-one (one-on-one) training, we will maximize your abilities tailored to each individual.
Physiotherapy
Exercise therapy (joint range training, strength enhancement training, balance practice, movement practice, walking practice, etc.), orthosis therapy, and physical therapy enhance exercise and movement ability and promote improvement of disability.
From 2016, we started walking practice using robots with the aim of improving the efficiency of walking and helping to improve the amount of activity.
Exercise therapy

Individual medical care
The exercise therapy room is a wide and bright space facing the courtyard. Sitting, standing, walking, etc., using a circle-shaped walking path of 50m per lap, 16 beds placed in a spacious space, 8 parallel bars, etc. Perform basic movements such as walking with a physiotherapist one-on-one (one-on-one) with a physiotherapist.

Group medical care
As a dynamic balance practice, we conduct group practice by multiple patients and physiotherapists.
The practice program is selected with original content that combines rehabilitation sports and compound movements according to the motor function of the group members.
We also incorporate group medical care, in which multiple patients provide common programs aimed at improving balance and walking durability. Utilize orthoses and wheelchairs according to the patient's condition to achieve independence in daily life activities.
We will provide movement practice, voluntary practice, and assistance method guidance according to your life after discharge.
Rehear courtyard
The outdoor rehabilitation courtyard, which is directly out of the rehabilitation floor, has three slopes with different slopes and outer stairs, in addition to a block-paved space of 700 m2 on the site. In an open and safe space, outdoor walking practice such as irregular walking and applied walking is possible.
Walking robot

Walking practice using robots
We are working on advanced walking practice using walking robots. By using a walking robot according to the patient's walking ability, we aim to improve the ability to walk faster and longer.
Voice of Users
"You put your right foot forward. I'm glad I used it."
"I think it has led to speed and endurance."
"I don't think it's easy to walk when it's heavy. It's easy to walk after removing it."
"The knees come forward. I got used to putting my feet straight."
Orthosis therapy
Bracelet
We have various types of equipment as equipment, and practice using equipment according to the stability of physical function and movement.
Wheelchair
Wheelchair
We have a large number of adjustable wheelchairs and wheelchairs with reclining functions. Select according to the patient's physique and physical function, and if you need a wheelchair to move, please use it exclusively during hospitalization. The therapist adjusts according to the posture and movement of each patient to improve function.
Occupational therapy
This section introduces physical exercise activities, daily life activities, life-related activities, and SPIR-IT work activities carried out by occupational therapy at our hospital.
Physical exercise activities
Physical exercise activity is a work activity that aims to improve basic posture and movement, such as sitting and standing, and to improve the range of motion, muscle strength, and skill of the paralyzed upper limbs.
Sitting training
I practice moving to reach a distance using a ring and pole and sitting balance.
The patient is reaching out to the pole ahead and moving the ring of the ring toss while maintaining a sitting balance.
The occupational therapist sits on the patient's paralyzed side and supports the paralyzed arm so that the patient does not fall down.
Electrical stimulation
The patient puts a free exercise-assisted low-frequency therapy device on the forearm and holds the beanbag on the table.
By using this treatment device, you can support your muscle strength and operate, and by practicing repeatedly, you can gradually increase muscle strength.
Upper limb robot-type exercise training equipment
Using the upper limb robot-type exercise training device called Reogo-J, we practice according to the range of motion and muscle strength of the paralyzed upper limb.
Occupational therapists create and train tailored programmes from patients with severe paralysis to relatively mild patients.
Using Reogo-J, patients can now practice more independently.
Leather work
Occupational therapy uses various craftwork for treatment mainly as practice such as muscle strength of upper limbs and fingers and skillful operation.
This is one of them.
Leather work can be done while having fun as an original work, and it is also appreciated as a gift for yourself and your family.
Origami
Origami is also one of the craftworks used for treatment.
It is also used as a practice of skillfulness of fingers, and as a procedure-based three-dimensional assembly work, as an issue for visual perception and performance dysfunction in higher brain dysfunction.
You can enjoy the finished product.
Daily life activities
Daily life activities include eating, dressing, excretion, changing clothes, bathing, etc.
We will support activities that have become difficult due to illness or injury safely and easily.
Chopstick movement
I practice eating.
In the photo, I practice picking with a springed chopsticks (chopsticks shaped like tweezers) with a paralyzed hand.
Changing operation
I also practice changing clothes.
I sit on the bed and practice putting on and taking off my jacket.
I practice introducing how to wear such as passing through the sleeves and hem from limbs that are paralyzed and difficult to move.
Shoe shoes
I wear socks using a self-help tool called Sock Aid.
This is used for those whose hip joints are not bent enough and bent forward and cannot reach their toes.
Bathing operation
In the photo, I am training in the bathroom to enter and exit the bathtub. When entering and exiting the bathtub, the body is supported so that the occupational therapist does not fall in and out of the paralyzed feet while sitting on the edge of the bathtub.
Life-related activities
Life-related activities refer to housework and social activities other than daily life activities.
Cooking training
In the kitchen, a patient is cutting carrots with a kitchen knife with his left hand.
Occupational therapists are watching behind the patient.
Dry laundry
I dry my laundry such as a towel on a pinch hanger.
Occupational therapists are watching with some help.
Cleaning
I clean the floor with a simple mop.
The paralyzed hand also has a mop handle.
Occupational therapists are watching and talking about how to use paralyzed hands.
SPIR-IT/HANDS therapy (HANDS: Hybrid Assistive Neuromuscular Dynamic Stimulation)
In our hospital, we are working on YOKOHAMA SPIR-IT for HAND (Yokohama Spirit for Hand).
This is a program that provides upper limb function training with the goal of hands that can be used in daily life for those who have left paralysis after a stroke.
SPIR-IT refers to Self-Propelling Improvement and Recovery Integrated Therapy (improvement and recovery promoted by oneself, integrated training for that purpose), and is an acronym called SPIR-IT.

Voluntary exercise assistance type electric stimulation device
SPIR-IT incorporates HANDS therapy (HANDS: Hybrid Assistive Neuromuscular Dynamic Stimulation), a therapy that promotes paralyzed hands by applying electrical stimulation using a device called "voluntary exercise assistance type electric stimulation".
Inspection
We carry out various tests to check where and how much paralyzed fingers and arms can be moved.
Use hands in daily life
When you have a stroke, you often have to do something with one hand, which used to be done with both hands as usual.
In accordance with the function of the patient's hands, we will set specific goals as hands that can be used in daily life, and practice actually using them in daily life.
The photo shows a toothbrush with a paralyzed hand and a toothpaste.
Voluntary training
Occupational therapists create voluntary training tailored to the patient's hand functions and goals.
If necessary, use low-frequency therapy equipment and robot training.
In the photo, I wear an assisted low-frequency therapy device on my paralyzed arm and practice pinching and moving objects.

Individual training
In individual training, we check daily progress of voluntary practice and how much paralyzed hands can be used outside of the training room.
In this context, we will set new goals according to the achievement status of the goals, add voluntary training, and adjust the difficulty.
Speech and hearing therapy
We provide specialized services to those who have problems with communication due to cerebrovascular disorders such as cerebral hemorrhage and cerebral infarction, or who have difficulty eating or swallowing, so that they can send a fulfilling daily life I am.
Currently, 11 speech therapists have been conducting rehabilitation since the acute phase immediately after onset.
Aphasia
Cerebrovascular disorders, etc., have impaired language functions such as listening, understanding, speaking, reading, and writing.
Various symptoms appear, such as the difficulty of seeing what you think, saying the wrong language, and hearing but not understanding the language.
In addition to starting evaluations and training early on the onset of the disease, we regularly hold "family courses" so that families who support patients can understand aphasia and communicate effectively.

Training in speech and hearing therapy
Speech therapists and patients often sit across desks, and train while watching them so that they can concentrate and relax according to the situation.
Aphasia test
This is a scene where a patient with aphasia chooses pictures.
Aphasia can cause "hearing understanding" disorders, which are difficult to accurately understand what the other person has said.
In order to find out how much hearing is possible, a speech therapist communicates words and sentences by voice, and implements a problem in which patients select pictures that match the words from several. Where you are.
Aphasia family course
The booklet in this photo summarizes the questions and answers received at the "Aphasia Family Course" held once a month at our hospital.
Handed to applicants, such as families who participated in the aphasia family course.
In addition to explanations to deepen your understanding of aphasia, there are questions and answers from your family through the course, such as "What should I do in such a case?"
※Family courses are suspended in 2024, and are undecided in 2025.
Syntax disorder
If motor disorders such as paralysis occur in the vocal organs such as vocal cords, lips, tongue, and soft mouth, various symptoms appear in the voice and pronunciation, such as poor voice, unclear pronunciation, and changes in speaking speed. You. We provide exercise training for vocal organs such as the mouth and tongue, breathing and vocal training, accurate pronunciation training, smooth speaking training, and guidance on effective communication methods.
Eating and swallowing disorders
Symptoms such as not being able to chew food well, being unable to feed into the throat, and coughing frequently occur.
As swallowing evaluations, video swallowing imaging (VF) and swallowing endoscopy (VE) are also conducted. We examine VF and other test results, and conduct throat and mouth exercise training, swallowing training, etc.
In addition, we observe meal scenes and cooperate with other professionals to provide guidance on safe eating and appropriate dietary content.
Check for dysphagia
In this photo, I'm checking the movement of swallowing with my fingertips on my throat.
When swallowing food, exercise occurs from the bottom of the chin to any lower side.
We check whether the exercise is being carried out at the appropriate timing and size by lightly applying the fingertips to the throat.
Tools used in evaluation of swallowing disorders
These are tools used in tests and training for dysphagia.
There are four disposable tools on the paper cup, which are lined up from the left side with "cotton swabs", "tongue pressure", "syringe", and "spongage brush". "Syringe" is a so-called syringe container that is used to weigh and put it in the mouth when drinking a small amount of water.
Other things are used to clean the mouth and to make it easier to observe the inner side of the mouth.
The one in front of the photo is a commercially available jelly. It is made to make it easy to swallow and hard to get stuffy.
When you haven't eaten it for a while, you will first eat such commercially available jelly or jelly made at our hospital, and evaluate how much you can eat it.
Psychotherapy
Cerebrovascular disease is a disease in which the brain, which is the human control tower, is damaged. As a result, various symptoms may occur depending on the location and spread of the damage, and may remain as a disorder. Disorders include physical functions such as exercise and sensation, as well as acknowledgement functions such as attention, memory, perception and language. A sudden illness can also cause instability, such as sinking or irritating, and may not be ready for rehabilitation. The certified psychologist of our hospital works on cognitive impairment and feelings other than language among the above. To put it simply, it can be said that it is a job that is responsible for mental and head rehabilitation. In addition, I am in charge of psychological tests for forgetful outpatients and forgetful docks.
Just a disability
Find out what damage has occurred due to brain damage and convey the results. Methods include conducting various psychological tests to detect disabilities, interviewing and behavioral observation.
Cognitive training
Encourage awareness of disability and think together about how to deal with it.
In some cases, issues may be implemented to reduce disabilities, and we may discuss how to deal with them in daily life.
In some cases, people with similar disabilities may be gathered and trained in groups.
Psychological counseling
By providing a place to express emotions freely and speak inner words, we help you organize chaotic emotions and face yourself today.
In addition to counseling through dialogue, we may also use a method of setting specific action goals to focus more on behavior than feelings, or a method of drawing or expressing the inner surface in a miniature garden.
Psychological Room
You can talk in an environment where the privacy of patients and their families is protected.
Discharge guidance and outpatient follow-up to achieve rapid return to society
Toward discharge
In addition to voluntary practice and guidance on how to assist caregivers according to their lives after discharge, we also provide consultation on welfare equipment and living environment improvement.
Practice standing from the floor
Assuming a Japanese-style life after discharge, we practice sitting on the floor and standing from the floor, which is the most difficult operation for patients with paralysis, in a real tatami room.
In order to avoid falls, we also teach family members how to assist.
Step up and down
For patients who go out in a wheelchair after discharge, we practice wheelchair operation and step up and down with their families, and provide guidance to ensure that they go out safely.
Outpatient follow-up
Currently, for patients with cerebrovascular disease who have been discharged from the convalescent rehabilitation ward to their homes, one month after discharge, for the purpose of grasping physical functions and living conditions after discharge, checking for assistive devices, etc. Follow-up is conducted outpatiently every two months and three months.
 Follow-up by a physiotherapist
Follow-up by a physiotherapist
 Follow-up by an occupational therapist
Follow-up by an occupational therapist
Rehabilitation of neurological disorders, etc.
Dizziness, spinal cord cerebellar degeneration, amyotrophic lateral sclerosis, Parkinson's disease, infectious diseases (encephalitis, meningitis), demyeling disease (multiple sclerosis), peripheral neurological disease (Gilan-Barre syndrome), muscle disease (muscular melanoma), metabolic disease (neurocomplication of diabetes), facial palsy, chronic subdialysis, chronic subdemia, etc.
Inquiries to this page
Yokohama City Apolexy and Spinal Nerves Center
Phone: 045-753-2500 (Representative)
Phone: 045-753-2500 (Representative)
Fax: 045-753-2859 (Representative)
Page ID: 285-231-849







